This blog post draws on two recent articles: When Sickness Interrupts Science” by Emily Sohn, published on www.nature.com on 10th Jan 2018, and Workplaces ‘should cater for menopause as they do for pregnancy’ by Hannah Devlin, published on www.guardian.com on 18th Jan 2018.
When sickness interrupts
A recent piece published on nature.com explores the challenges that sickness – by way of society’s response to chronic illness – can present in the workplace. With a focus on scientists with chronic health conditions, the article explores their illness experiences as they work to build their research careers. As an Associate Professor with chronic health conditions who is also working to build my own research career, the stories shared resonated with my own experiences and have prompted me to reflect on my own sickness interruptions.
So, how does sickness interrupt? Here’s where it’s important to really think about what is meant by sickness – how does it differ to thinking about illness and disease? Put simply:
- Disease refers to an identifiable pathogen that can be diagnosed by a healthcare provider, and is shown to cause poor health.
- Illness refers to the ways in which we, ourselves, experience poor health. This may, or may not, be due to the presence of a disease. Illness is about our own poor health experiences.
- Sickness refers to the ways in which others – society – understand and respond to our illness.
[If you’re interested, more about the sociology of health and the application of these concepts can be found here and here]
So when we’re thinking about how sickness interrupts, we’re really thinking about how society responds to our illness, and how this – in turn – mediates how we do (not) talk about our illness experiences.
My own research explores the ways that poor health interrupts daily lives. I’m increasingly interested in how chronic health conditions mediate our own illness narratives. Experiencing the ways in which my own health has interrupted my day-to-day has forced me to (re)think and (re)engage in a more involved and reflexive way in my own research practice, and to apply this to trying to better understand my own experiences (I’ve written a bit about this and autoethnography previously). My blog is one such way that I’m trying to more effectively – and creatively – write and reflect, and to balance interruptions (in multiple forms, not just health-related). I guess that this is an example of how my illness interrupts my research practice. Perhaps in a positive way.
My interruptions (aka my collection of chronic conditions):
- I have Hashimoto’s Disease (my thyroid was destroyed by my own immune system, resulting in hypothyroidism) and I take thyroid replacement medication daily.
- I was diagnosed with temporal lobe epilepsy (TLE) last year and I now take anti-epileptic medication twice daily.
- I had a diagnosis of borderline ovarian cancer (BOC), stage 2c in July 2014 and will have 6-monthly (and at some point 12-monthly) monitoring visits – ultrasounds, gynae exams, breast exams, blood tests – for the next 15-20 years [I guess this would make it a chronic health condition in some way].
- I’m experiencing surgical menopause as a result of a radical hysterectomy performed three and a half years ago when I was 35 and I have oestrogen patches that I change twice a week. [Whilst (surgical) menopause isn’t a chronic illness, it is a chronic condition – whether undergoing a surgical menopause or experiencing menopause in your 50s. Surgical menopause in your 30s isn’t fun: it happens overnight and it comes with a whole bunch of other possible health problems, including osteoporosis. Oestrogen replacement therapy is a life saver.]
When chronic health interrupts
Chronic health conditions do interrupt our lives in multiple ways; they interrupt our careers, our families, our friendships.
Whilst our colleagues, our families, and our friends are often supportive (mine most certainly are), it doesn’t (re)solve the (potential) challenges we face daily.
Acknowledging that a chronic health condition is now affecting our lives day-to-day isn’t easy. It is difficult to recognise that our own work – whatever that may be, whether it’s work outside the home, as a parent, as a carer for others, as a CEO – is now affected in unexpected ways. The ways we experience our illness and the ways in which others respond to our sickness impact our daily lives.
Julia Hubbard, a biophysicist who has type 1 diabetes and the autoimmune disease lupus
It’s a confusing space to be in.
I’m often frustrated, and angry.
And then I remember to breathe and I remember to be proud of what I’ve achieved over the last few years. But then I’m frustrated and angry – a sentiment shared by Jennifer Mankoff, a scientist who was diagnosed with Lyme Disease:
I’m all too easily frustrated and angry.
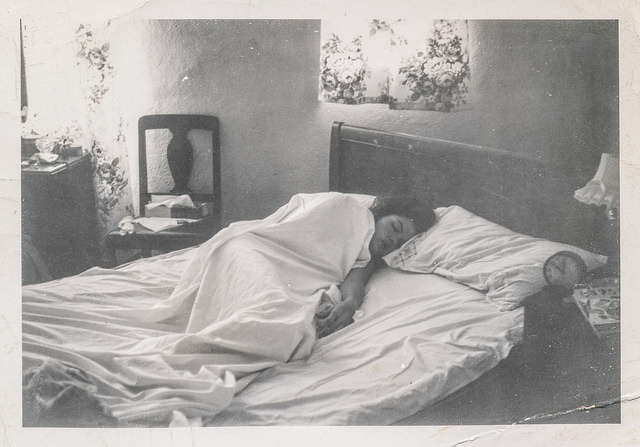
I’m frustrated and angry that my brain doesn’t work like it used to. I’m frustrated and angry that I forget things and miss deadlines, appointments, and friends birthdays. I’m frustrated and angry that I can’t juggle as many balls as I used to be able to and struggle to manage multiple things at once. I’m frustrated and angry that I get hot flushes and super angsty when I forget to change my oestrogen patch. I’m frustrated and angry that when I forget a dose of my anti-epilepsy meds – even by a few hours – my brain goes upside down and I experience vertigo and other strange things. I’m frustrated and angry that I have to remember to refill my prescriptions on time every month and that when I travel I have to fight with my medical aid to get early refills. I’m frustrated and angry that when I don’t practice #selfcare I run out of steam, and feel shit and exhausted and anti-social. I’m frustrated and angry about moments of self-sabotage when I skip my meds, or can’t face another trip to the pharmacy. I’m frustrated and angry about how mental exhaustion from my trippy brain and broken thyroid, from hormone imbalances and the ever-present worry about a recurrence of BOC – or an occurrence of typical OC – means I need to take time out, to sleep, to lay low, and to have a duvet day(s) [this is brilliantly explained in the ‘spoon theory’, developed by Christine Miserandino].
But mostly I’m frustrated and angry about getting frustrated and angry. I’m incredibly fortunate. I have fast access to quality healthcare. I can afford my expensive medical aid, my expensive medication and my expensive medical procedures. I have chronic conditions that can – most of the time – be effectively managed through biomedicine and #selfcare practices. I had a diagnosis of borderline ovarian cancer, not of typical ovarian cancer. I have supportive family, friends and colleagues. As a result, I can work. I can live my life. I can find ways to manage the inconveniences and interruptions that these conditions bring. I can manage my illness experiences in ways that many cannot.
I have access to many resources but it isn’t always easy to resolve these chronic health interruptions.
For many, engaging with chronic health in the workplace is difficult:
When surgical menopause interrupts
I’m not sure if (surgical) menopause is recognised as a chronic condition but I think it should be. Whilst, for some women, menopause will be a temporary-but-chronic experience, for others it is a long-lasting experience. Surgical menopause is ever-present. In a recent article in The Guardian, Angela Bonnet – a senior finance manager – shares her experiences of navigating menopause in the workplace.
Health is personal. But it affects our day-to-day. How can we find safe spaces to share and reflect on the challenges that chronic conditions – including menopause, and, particularly surgical menopause – present to our day-to-day? How do we navigate this conversation in the workplace? How do we work to address the gendered nature of menopause and encourage our male colleagues to learn about this condition that affects 50% of the population. For me, I blog. And I do speak about my health and surgical menopause at work. But not with everyone. And not all the time.
But how can the ‘chronicity’ of menopause be dealt with in the workplace?
Whilst surgical menopause isn’t the same as going through menopause in your 50s, the message in a recently published piece on www.guardian.com is appealing: appropriate responses from the workplace – and wider society, please – are needed to ensure that women experiencing menopause are supported and not discriminated against.
But what responses are needed and how could these be managed in the workplace? ‘Menopausal leave’? A long period where opportunities to work via flexi-time are made possible? Reduced hours (with no impact on salary and benefits) or extensions on deadlines and regular tasks? Work-place interventions to support employees in sharing menopause-associated difficulties and needs with colleagues? Perhaps some kind of mix of the above: every woman experiences menopause differently. Some have a shorter period of symptoms, others experience symptoms for years. It’s exhausting. And many women feel embarrassed about experiencing hot flushes – and a host of other symptoms, including difficulties in navigating changing hormonal profiles and the impacts that this has on our brains – at work. Memory issues and other cognitive frustrations are common symptoms; it’s harder to concentrate and produce work in the way that we were able to do so before menopause.
I had 3 months off work after my radical hysterectomy; this was – with hindsight – about supporting my physical recovery from major surgery and didn’t actually give me a chance to engage with my hormones and bigger emotional issues associated with surgical menopause and such a sudden health crisis. Three and a half years later, it’s still something that I struggle with – although far less frequently now. I’m fortunate to have been able to have such a long period of sick leave and to be able afford to do so. My work means that flexibility is built in, which is a big help. But deadlines and responsibilities remain and, as my career grows, they keep increasing.
The challenge: to find ways to sustainably practice #selfcare in an already stress-filled world and workplace, around the added – and often unpredictable – challenges of surgical menopause, of BOC, of TLE, of Hashimoto’s.
When (can) we interrupt (?)
In terms of the workplace, it’s a tough one. And I think that the same sentiments also apply in our social and private lives. I’ve written about the challenges of not saying enough in order to protect others, and – at times – as a way to protect ourselves. But not feeling we can share our illness experiences is a heavy burden to carry.
#selfcare is key but I know I’m not the only one who struggles to enact self-caring interventions. The structure of the workplace can, often, overwhelm attempts to #selfcare – particularly when your brain and soul are already struggling. It’s a great idea and one I’m a believer in. But I’m super shit at practicing it.
We need to say and do what feels right, and we need to say and do what feels safe. Sadly, these are not always mutually exclusive and – as Mankoff says – there’s a fine line we have to navigate, particularly within the workplace: what can (should?) we say in order to access support and not criticism? How safe are our workplaces to discuss our long-term health-related needs? As a result of continued gender inequities in most workplace settings, women are likely to self-censor their illness experiences and long-term needs for fear of being further discriminated against. And this, in itself, makes me frustrated and angry. Again.
Image: https://www.flickr.com/photos/simpleinsomnia/24912557863/
If you’re an academic with chronic health conditions, join the Chronically Academic community. I’ve just discovered it. And wish I had done earlier.

Leave a comment